More than 44,000 corneal transplants are performed in the United States each year.
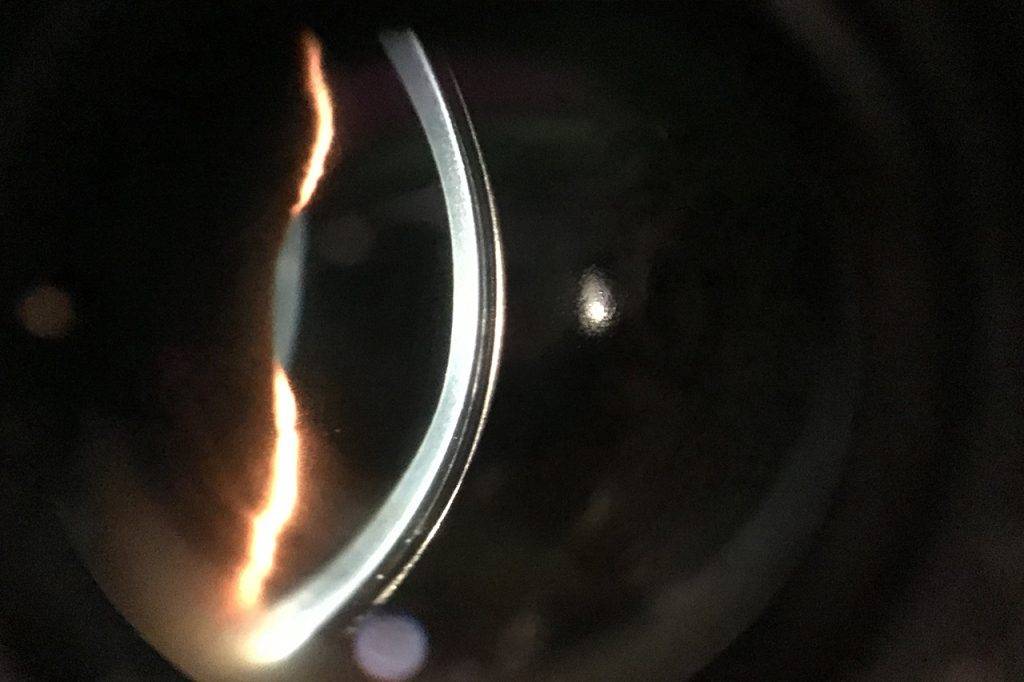
The cornea is the outermost layer of the eye that is responsible for protecting the eye and bending light as it enters the eye, a vital first step in the process of vision.
In a healthy eye, the cornea is clear and dome-shaped. However, when the cornea becomes damaged from an injury or corneal ulcers, its shape and transparency can be affected— impacting its ability to bend light in an effective manner.
When this occurs, light cannot be accurately focused onto the retina, and the image we see appears blurry or distorted.
What is a corneal transplant?
A corneal transplant, also referred to as a keratoplasty or corneal graft, involves replacing the damaged or diseased area of the cornea with healthy corneal tissue received from a donor.
In some cases, if a donor cornea is unavailable, an artificial cornea, called a keratoprosthesis, may be implanted instead.
This surgical procedure is used to treat severe corneal damage or infection, relieve pain, and improve vision.
When is a corneal transplant recommended?
Corneal transplants may be recommended for a number of different corneal conditions.
The highest number of transplants are performed on patients with keratoconus.
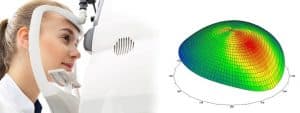
Keratoconus is a condition that causes the dome-shaped cornea to alter into an irregular cone shape with a pronounced bulge. This condition can cause significant vision impairments.
A corneal transplant may also be recommended for the treatment of:
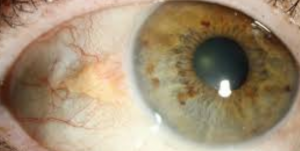
- Corneal ulcers (keratitis)
- Corneal perforation
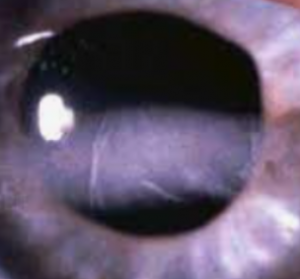
- Corneal scarring
- Corneal swelling
- Clouding of the cornea
- Thinning of the cornea
- Corneal stromal dystrophies
- Fuchs’ dystrophy
- Bullous keratopathy
- Viral or bacterial infection
- Corneal complications following eye surgery
If you suspect you have an eye condition, contact an eye doctor near you, who can diagnose and treat the condition.
SEE RELATED: Corneal Ulcers
Types of corneal transplants
There are three different types of corneal transplant procedures. Each procedure involves the replacement of a different area of the cornea:
- Penetrating keratoplasty (PK): This is the most frequently performed procedure. During a PK procedure, the entire thickness of the cornea is replaced. The corneal surgeon will use a laser or surgical instrument to cut out a circular shape from the damaged cornea. A donor cornea with a matching circular shape is then sutured into place.
The sutures remain in the eye for approximately one year, and total vision improvement may not be noticed for around 18 months. In the meantime, your eye doctor may recommend wearing corrective eyewear for improved vision.
- Deep anterior lamellar keratoplasty (DALK): During a DALK procedure, also called a partial thickness transplant, only the outer and middle layers of the cornea are replaced or reshaped. This type of transplant is often performed for keratoconus treatment.
With this procedure, improved vision is generally noticed within just a few months of the surgery, as the recovery time is shorter than the PK procedure. The DALK procedure has also shown a reduced risk of donor tissue rejection, when compared to the PK procedure.
- Endothelial keratoplasty (EK): During an EK procedure, only the deep, back layers of the cornea are replaced. This procedure is used for certain corneal conditions such as Fuch’s dystrophy and corneal swelling, that affect the endothelium layer of the cornea, which is responsible for maintaining fluid balance within the cornea.
During this procedure, the damaged endothelium layer of the cornea is replaced with donor endothelial tissue, leaving the healthy outer corneal layers intact. An air bubble is used to measure correct positioning. Sutures are not needed for this procedure, as the small incision will heal on its own.
The most frequently performed EK procedure is called Descemet’s Stripping Endothelial Keratoplasty (DSEK). The DSEK may even be superior to the PK procedure, as it provides optimal visual results with fewer risks of complications.
The EK procedure is known for its faster recovery of vision with a reduced risk of astigmatism, minimal removal of corneal tissue, and faster operation time, without the need for sutures.
Patients who undergo this type of procedure usually notice improved vision within a few weeks to a few months.
How effective is corneal transplant surgery?
The majority of corneal transplants are successful, facilitating improved vision for most patients.
According to research, 95 percent of PK procedures performed for keratoconus and other low-risk conditions, lasted for 10 years or more.
Are corneal transplants safe?
A corneal transplant is a relatively safe procedure, though like any other surgery, it carries a risk of complications.
The most frequent complication from a corneal transplant is rejection of the donor cornea, occurring in about 10 percent of corneal transplants.
This can occur when the body’s immune system does not recognize the new tissue and therefore attacks the foreign matter.
If this occurs, your eye doctor may prescribe a medication to help the body to accept the new tissue, or recommend a second corneal transplant.
Other complications can include:
- Eye infection
- Swelling of the cornea
- Cataract– clouding of the eye’s lens
- Glaucoma– increased eye pressure
If you experience any of these symptoms following your corneal transplant, contact your eye doctor’s office as soon as possible:
- Vision loss
- Eye pain
- Red eyes
- Increased light sensitivity
Corneal transplant complications and rejection continue to be a risk for many years following the transplant procedure. It is therefore essential to keep up with your scheduled eye exams, according to your doctor’s recommendations, and inform your doctor of any visual changes since your last visit.
Recovering from a corneal transplant
For optimal results, practice these eye health and safety guidelines, as well as any other directions given to you by your eye doctor following your corneal transplant:
- Take your medications as prescribed to prevent infection and reduce pain and swelling.
- Avoid activities that can cause an eye injury or contamination such as contact sports, exercise, and swimming.
- Avoid rubbing your eye.
- Wear an eye patch as directed by your doctor.
- Schedule follow up eye exams according to your eye doctor’s recommendations.
Adjustments to improve vision
Once your eye doctor has determined that your cornea has healed from the transplant, adjustments can be made to further improve your vision.
Astigmatism. If the stitches that are holding your new cornea in place are causing an irregular corneal shape and astigmatism, your eye doctor can adjust your stitches until the desired corneal shape is achieved.
Refractive errors. To correct blurry vision from nearsightedness or farsightedness, your eye doctor can prescribe an optical prescription for eyeglasses or contact lenses, and may even recommend laser eye surgery.
Corneal transplants are the second most common type of transplant, after blood donations.
If you have any questions or concerns about corneal transplants, speak with an eye doctor.
LEARN MORE: Guide to Corneal Diseases
Schedule an appointment with an eye doctor for a comprehensive eye exam, and to discuss any questions you may have about your eye health.
A corneal transplant could provide clearer vision, for an improved quality of life.